Kellie Burns spent much of last week asking urgent and personal questions of total strangers. Sitting cross-legged on her bed in Baltimore, in text after Facebook message after phone call, she pressed: When did you test positive for COVID-19? How long have you been feeling better?
Kellie wasn’t trying to socialize. She was just trying to save her father’s life.
Bill Burns was admitted two weeks ago, on Tuesday, March 31, to the intensive care unit at the Glens Falls Hospital in upstate New York, where he tested positive for the coronavirus. Bill, 62, had struggled with respiratory problems ever since working as a steamfitter on the post-9/11 Ground Zero cleanup. On Wednesday, he was put on a ventilator. On Thursday, Kellie asked her father’s doctors to get him a transfusion of convalescent plasma. Kellie, a former health care consultant who’d been tuning into New York Gov. Andrew Cuomo’s daily coronavirus briefings, had determined that the experimental treatment was the least risky, most feasible option to give her father a fighting chance.
Plasma therapy is a century-old medical practice that involves transferring the antibody-rich part of the blood, a yellowish liquid called plasma, from people who have recovered from a disease into those struggling to fight it off. It was used in the early 1900s to treat measles and mumps, and, more recently, to treat other coronaviruses, like MERS and SARS. Early outcomes from patients in China suggest that it could serve as a treatment for COVID-19, though, as Dr. Arturo Casadevall, an infectious diseases expert at Johns Hopkins University, explained, the “coronavirus is a new virus, and whenever you’re dealing with a new entity, you need testing.” In early April, the Food and Drug Administration unveiled a national study to test those interested in receiving the experimental treatment. Under the best-case scenario, plasma could treat sick patients while a longer-term therapy, like a vaccine, is developed.
Of the treatment options floating around in the news, plasma is the only therapy that has been used for decades and is known to be relatively safe, says Casadevall. Plus, it can be implemented quickly because it doesn’t require any drug development: Theoretically, the beneficial, virus-fighting antibodies exist in the blood of most people who have recovered from the coronavirus.
The problem is, “We don’t have an infrastructure for convalescent plasma,” says Casadevall. “It is being developed as we speak.”
In recent weeks, an alphabet soup of public health organizations, including the FDA, the Red Cross, and the American Association of Blood Banks (AABB), has come together in an attempt to quickly build a national plasma supply from scratch. The mobilization is unprecedented in scope, requiring the coordination of hundreds of hospitals and blood centers, and thousands of prospective donors and patients. But the process has been off to a clunky start, in part because there’s no clear person or group in charge. “People talk about the blood supply as though there’s a single national blood system, which there isn’t,” said Eduardo Nunes, the AABB’s vice president of quality and standards. “There isn’t a single, centralized point of decision making to the entire community.”
For now, the plasma supply is minuscule: Plasma needs to come from people who tested positive for the coronavirus and haven’t exhibited symptoms for weeks, in addition to meeting the typical criteria for blood donation, like having enough iron and not being on certain medications. Blood banks across the country are in the early stages of soliciting donors. “It’s very frustrating for me to have to tell people, ‘I’m sorry, but we don’t have it yet,’” said Dr. Louis Katz, the acting chief medical officer at Mississippi Valley Regional Blood Center, which has locations across the Midwest. “We’re building an airplane as we fly.”
As a result, families like Kellie’s are left with few options. Some are starting to plead with medical professionals—on Thursday, Katz received phone calls from three doctors representing desperate families in just the 20 minutes before we talked—while others are turning to social media and local news outlets in search of donors for their loved ones. Survivor Corps, a Facebook group with more than 30,000 members, functions as part support group for COVID-19 patients and their families and part grassroots plasma donor network, with pleas from family members across the country looking for donors and specifying the blood type they’re looking for. The messages are equal parts devastating and inspiring. “My husband is currently fighting for his life, on a ventilator, in the ICU,” read one post on Sunday. “Please help if you are able. This disease is nasty and terrifying.”
On Tuesday, another woman wrote, “Hey my doctor just called and said I am free of covid!!!” She continued, “Now how can I go and donate my plasma in Los Angeles. Anyone know? I would love to help as many people as I can.”

Glens Falls is a small hospital, and Bill Burns was among the first coronavirus patients admitted to its ICU. When Kellie first spoke with his doctors and nurses over the phone from her home in Baltimore—like other hospitals, Glens Falls has shut down access to visitors—she felt the staff weren’t responsive to her pleas. “They’re frantically trying to figure out what the best things are, too,” she told me.
So Kellie took matters into her own hands. She started reading up on the FDA process for getting plasma from donor to patient. On Saturday, April 4, Kellie finally connected on the phone with hospital staffers who had a moment to spare, who then contacted the FDA and the American Red Cross about getting plasma for Bill. An email from the American Red Cross to Bill’s pulmonologist explained that the organization was in the process of building up a plasma inventory, but things were still very preliminary. In the meantime, it read, “We need the hospitals’ assistance to find an appropriate donor.”
In other words, if Bill was going to get plasma, someone else was going to have to find it.
Kellie knew that plasma was no panacea. “What’s weird about this is, you’re fighting hard for something that could have no effect,” she told me last week. “All you can do in this situation is make sure you don’t have any regrets about how you tried to help your loved one.”

Bill Burns with Kellie’s daughter, Hazel
Kellie Burns
On Sunday, Kellie took to Facebook: “Our father is still in critical condition with COVID-19 and after speaking with his doctor, we believe that plasma from a recovered patient is his next best treatment option. The problem is, WE NEED A DONOR!” The post was shared nearly 300 times in three days, and Kellie started getting texts, calls, and emails from strangers who wanted to help—so many that Kellie and her five siblings were having trouble keeping up. On lively family video chats—“I’m from very loud, big Italian family,” Kellie explained—they shared regular status reports from the hospital and donor leads.
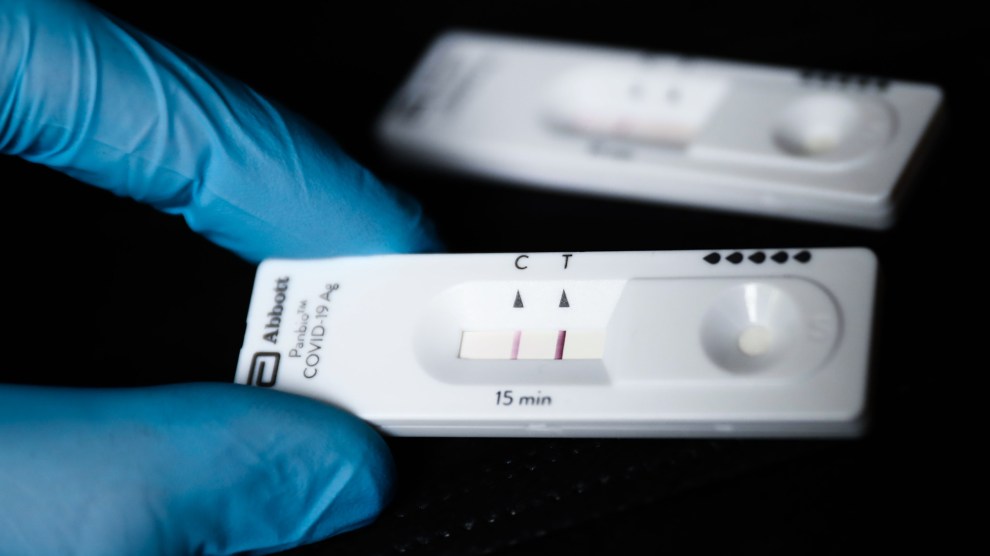
According to FDA’s rules, donors have to be symptom-free for at least two weeks and test negative for the coronavirus, or be asymptomatic for at least four weeks. (Eventually, prospective donors may have to take antibody tests, but for now, the accessibility and accuracy of such tests are too limited.) Some of the people Kellie talked to had been diagnosed with the coronavirus by a doctor but never got the official positive test. Others had trouble getting the second test to show they were negative. Given the short supply of diagnostic tests, it seemed virtually impossible to know who had viable plasma, particularly if they were under the 28-day mark. “That is one of the big stumbling blocks at the moment to opening the taps as wide as we possibly can,” said Dr. Claudia Cohn, chief medical officer of AABB.
People whom Kellie had never met before went to extreme lengths to help. One complete stranger in Chicago offered to get on a plane and fly to Albany to donate her plasma for Bill. Another drove from New Jersey to Manhattan during his lunch break after Kellie learned that the New York Health Department would be testing some ConEd workers for the coronavirus that afternoon and had one extra test to spare. A third prospective donor, a nurse in Glens Falls named Tony, drove three hours to Syracuse to get tested.
“It’s unbelievable how kind people have been, how much they want to help,” Kellie said.
But five days after her call for plasma, after being glued to her phone while her husband took care of their 15-month-old daughter, Kellie was still out of luck. “Long story short, we don’t yet have a qualified donor,” she wrote on Facebook on Friday, April 10. “We had 3 very promising candidates as of this morning, but by 8pm all 3 had been disqualified.” One didn’t have the right kind of testing; the other two had once again tested positive. Her father was still alone in the ICU, sedated on a breathing tube, and running out of time.
Meanwhile, Kellie was noticing more and more petitions on social media asking for plasma. “It’s getting to the point where you see it and you’re like, this is just silly,” she told me. “It can’t be this way—where people are looking for individual donors.”

It’s not supposed to be this way. In theory, any hospital that is enrolled in the FDA’s new Expanded Access study, which is run by the Mayo Clinic, will soon have access to an inventory of plasma available at local blood centers—a process similar to how blood is managed. That way, people like Kellie won’t have to solicit direct donations, and the system won’t give preference to families who have the resources to advocate for themselves.
Usually, hospitals have to work through layers of red tape to participate in federal investigative studies, but the FDA waived many of the usual rules to fast track the plasma donation process: Hospitals and doctors interested in plasma transfusion simply fill out a few online forms. Glens Falls Hospital enrolled in the study last week, on Bill’s ninth day on the ventilator. Since the registration website went live 12 days ago, more than 1,000 hospital sites have signed up to participate.
A steady supply of plasma is likely weeks away, experts say. As of Tuesday, 118 patients had received plasma transfusions through the Mayo Clinic study. The American Red Cross collected plasma from just five donors last week, producing 15 units of convalescent plasma, each of which can help one person. In hard-hit New York, hundreds of donation registrations have come into New York Blood Center since Gov. Cuomo encouraged coronavirus survivors to donate plasma during his press conference last week. But as of Friday, the center, which was among the first in the country to get a donation program up and running, and which provides nearly all the blood to hospitals in New York City and the Hudson Valley, only had enough plasma to reserve two units per hospital. New Yorkers will “certainly be the source of a lot of plasma in coming weeks and months” as other regions hit their peaks, said Katz. “It’s unfortunate that we can’t just turn on the spigot, but it’s also true.”
In the weeks to come, while plasma demand outpaces supply, blood banks, hospitals, doctors across the nation will face thorny questions: Who deserves this experimental treatment? If a patient’s family finds a donor for their loved one, should that donation actually be directed to the patient? What happens to the many families who don’t have the time or resources to take to Facebook and reach out to local news channels? Then, there’s the question of severity: Evidence suggests that those who are earlier along in the disease will benefit more from plasma than those who have progressed and are much sicker, says Cohn. But “ethically, you feel like they deserve every treatment that’s available,” she says. “That’s going to be a very difficult call to make. The collective hope is to get to a point where the supply where we’re no longer dealing with this.”
Katz, for one, told me on Thursday that since going live with its convalescent plasma collection last week, the Mississippi Valley Blood Center had so far identified one potentially eligible donor. I asked how he was going to decide which three lucky patients would receive it. He groaned, said, “Oh, Lord,” and added, “I think it’s going to be first come, first serve. I mean, am I supposed to decide who’s too sick and not sick enough? I don’t think that I’m qualified to do that—or anybody else is.”
On Saturday evening, during a group FaceTime with her family, Kellie got a call from the hospital. It was her father’s doctor. She got straight to the point: “Your dad is about to get the plasma transfusion.”
While Kellie had been pleading with strangers, the system worked as it was supposed to: A recovered coronavirus patient in Long Island donated plasma to New York Blood Center’s nascent inventory, and Glens Falls Hospital, equipped with its FDA study enrollment, had put in a request for plasma. Miraculously, Bill Burns got one of the few doses in stock. On Saturday afternoon, a courier drove the blood three hours from Long Island to Glens Falls.
“WE DID IT!!!” Kellie wrote on Facebook on Saturday evening. “Thank you to every single person (and there were many!) who made this a reality. It was totally unexpected and it didn’t happen the way we thought it would, but it happened. I will definitely share more details later, but for now I am going to sleep!”
When I spoke to Kellie on Sunday, the high had worn off a bit. If the plasma transfusion works, it will likely take two to three days to show any effect, leaving the Burns family in an anguished waiting game.

The Burns family during Christmas of 2019
Kellie Burns
On Sunday, they learned that Bill had developed a bacterial infection, which is common for patients intubated for long periods of time. By that point, the Burns family hadn’t laid eyes on Bill for 12 days, and the nurses offered to hold up an iPad so the family could talk to him. On the screen, Bill had a tube hanging out of his mouth. The drugs had stilled him. Kellie could almost pretend that he was just sleeping. The faces of the Burns kids and their mother filled the screen, but no one knew quite what to say. Kellie’s mother tearfully said “I love you” over and over, adding that their two dogs missed Bill, too. Bill is a big sports guy—he’d coached his sons’ football teams—and on the phone, the now-grown sons told their father to keep up the fight.
The call lasted just four minutes. “There’s only so much you can say, right?” Kellie told me afterwards, sounding exhausted. “You’re just hoping that they hear your voice. Even that just feels enormous at this point.”
Those who are interested in donating plasma can find more information on the AABB website.