An anxious man on the phone.Craig F. Walker/Getty
This story is from Columbia Journalism Investigations and the Center for Public Integrity, a nonprofit, nonpartisan investigative media organization in Washington, D.C.
In late August 2017, Hurricane Harvey cut through Texas and other southern states, its catastrophic floods affecting millions of Americans. Within a month, Hurricane Irma swept through Florida, and then Hurricane Maria devastated Puerto Rico.
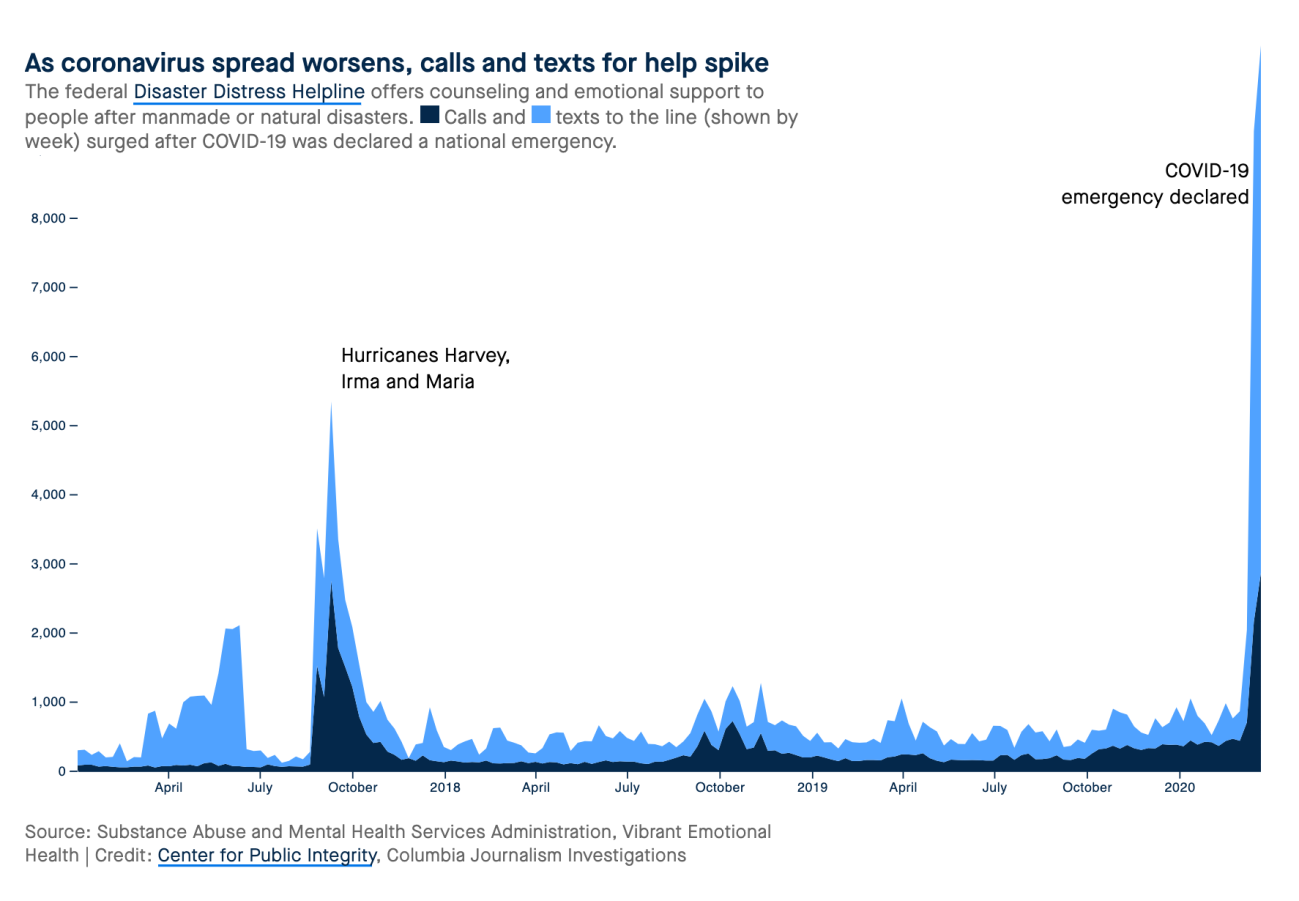
The federal Disaster Distress Helpline saw a surge in calls and texts for help that September. Nothing since has topped that—until now.
The helpline, 800-985-5990, run by the Substance Abuse and Mental Health Services Administration and the nonprofit Vibrant Emotional Health, answered roughly 7,000 calls and received 19,000 text messages in March, a more than eight-fold increase from February. That far outstrips the number of texts and calls in August and September 2017 combined, according to data obtained by the Center for Public Integrity and Columbia Journalism Investigations.
Amid the coronavirus pandemic, hotlines in the US are seeing a spike in activity that might be unprecedented. That’s because the situation is, too.
“This feels different, and it is,” said Roxane Cohen Silver, a professor of psychological science, medicine and public health at the University of California, Irvine. “This is an invisible threat: We don’t know who is infected, and anyone could infect us. This is an ambiguous threat: We don’t know how bad it will get … we don’t know how long it will last. And this is a global threat: No community is safe.”
Dozens of studies link psychological burdens with isolation and crises, including epidemics. In one study of Hong Kong’s 2003 severe acute respiratory syndrome outbreak, nearly half of surveyed residents said the experience weighed on their mental health. Sixteen percent showed signs of post-traumatic stress disorder, or PTSD, six months after the outbreak ended.
Sarah Lowe, a psychologist and assistant professor at Yale School of Public Health, calls the coronavirus a “slow-motion disaster” with potentially widespread and persistent mental-health fallout. Lowe, who studies the effects of disasters, said she worries that some people will be disproportionately affected, particularly medical workers, the sick, those with pre-existing mental illness and anyone facing economic challenges.
“We know from previous disasters that long-term financial strain tends to be associated with depression and PTSD,” she said.
Like the federal hotline, the National Alliance on Mental Illness’ HelpLine is seeing a surge in calls. Before COVID-19, the illness the novel coronavirus causes, 150 calls would be a big day, said Dawn Brown, the HelpLine director. Now it’s surpassing that number daily.
“It’s continuing to go up,” she said, adding that nearly half the callers at some point mention the virus.
Callers to NAMI’s line, 800-950-6264, are sharing feelings of anxiety and depression as well as asking for advice about how to continue mental-health treatment and get medicine refilled during stay-at-home orders.
“People with mental illness require a great support system,” Brown said. “They don’t do well with uncertainty and ambiguity, which this has certainly caused. Just when you think you’ve got a handle on it, something else happens, whether it be a shelter-in-place order or more news coverage talking about death and shortages.”
In New York City, which has the most confirmed cases in the country, NAMI’s local affiliate is seeing jumps in calls to its own helpline, 212-684-3264. Call volume in the past few weeks has gone up roughly 60 percent, said Matt Kudish, the group’s executive director.
And the number of people taking a free screening test for anxiety offered online by the advocacy organization Mental Health America is up more than 20 percent from mid-February through mid-March, compared with the early part of the year. That’s the COVID-19 effect, said Paul Gionfriddo, the group’s president and CEO.
He’s worried the country may be under-reacting to the mental-health toll. “And it’s only going to get worse as we have to bring widespread grieving into the equation as more people die,” he said. “Because people will be grieving alone.”
Some federal and state health authorities are rushing to maintain psychological support. The US Department of Health and Human Services has expanded access to teletherapy, including for Medicare, and some states are waiving telemedicine restrictions for Medicaid. The US Drug Enforcement Administration is now allowing doctors to prescribe medications virtually without having to first meet a patient face-to-face.
New York Gov. Andrew Cuomo launched a COVID-19 Emotional Support Hotline, 844-863-9314, and said 6,000 mental-health professionals have volunteered to help.
What officials say in this fraught period also can help, or harm, mental health.
“Not every message from public health leaders will be comforting,” said Brian Hepburn, who leads the National Association of State Mental Health Program Directors. But consistent messaging will build trust, he said, and as a result “you are going to see a decrease in fear, in those spikes.”
The first uptick in calls to the Disaster Distress Helpline happened on March 16, the same day President Donald Trump announced recommendations such as closing schools and avoiding gathering in groups of more than 10 people. Six days earlier, he assured Americans that the administration’s response was “really working out” and downplayed the threat by saying deaths were minuscule compared with the flu.
Lowe said she was upset to see the president’s March 20 press conference, in which he criticized a reporter who asked, “What do you say to Americans who are scared?” Trump rebuffed the question, calling the reporter “terrible.”
“I found that invalidating of people’s fears and worry,” Lowe said. “People are afraid. Denying that will only make those feelings intensify.”
Two hotlines that aren’t seeing increased calls: the National Suicide Prevention Lifeline and the National Domestic Violence Hotline. Administrators at both are keeping a close watch for changes.
“Because we expect that people are spending more time at home, possibly not leaving the home for work each day, for example, we know survivors are spending more time in closer proximity to their abusers,” said Katie Ray-Jones, CEO of the domestic violence hotline.
Helplines and crisis hotlines are only an initial support system for people in emotional distress. Gionfriddo, of Mental Health America, is urging people — and elected officials — not to assume the anxiety and other corrosive effects will disappear on their own when the pandemic is over. The amounts of mental-health funding in Congress’ coronavirus package, he said, “are rounding errors,” money that in his view will not be enough to address the surge in needs.
“If we make them an afterthought—if we don’t address them aggressively—they’ll still be there,” he said.
Dean Russell is a reporting fellow for Columbia Journalism Investigations, an investigative reporting unit at the Columbia Journalism School. Funding for CJI is provided by the school’s Investigative Reporting Resource and the Energy Foundation. Jamie Smith Hopkins is a reporter and editor at the Center for Public Integrity, a nonprofit investigative newsroom in Washington, D.C.