Photo: AP/World Wide Photos
The creature arrived in the arctic as it had spread itself around the world. It lay dormant in the lungs of someone apparently healthy enough to undertake such a journey, and then, when he was weakened, perhaps by hunger, or cold, or simple loneliness, it revived itself explosively. The sailor, or the missionary, or the trader found himself coughing paroxysmally and febrile, in some little iglu or tent, the bacterium streaming through his blood, to all his organs, and then a local Inuk had the misfortune to enter the shelter and leave. In Arviat, one of the Inuit communities that hug the shore of Hudson Bay, lives a woman I will call Therese Oopik, who carries the descendants of the creature within her. I visit Arviat in my work as an internist and she is my patient. We have been acquainted for a decade. Mostly we have had quiet conversations about contraception and bladder infections; these days we talk about this infection that seems likely to claim her.
She was beautiful when I first knew her, with a full-faced smile and glowing from the cold, but for two years now she has lost weight steadily and she looks as emaciated as a New York City fashion model. We joke about this. When I next visit there, she suggests, I might find a job for her.
Arviat is populated by 1,800 people, almost all Inuit, and it clings to the low rocks that stretch into the Arctic water like a collection of brightly painted aluminum-sided mollusks. The wind scours this place. Everyone knows everyone else and most of their problems. There have been episodic outbreaks of tuberculosis here, as in all the little communities in this part of the Canadian Arctic, ever since that first coughing sailor or missionary arrived. Tuberculosis has smoldered on notwithstanding the advent of antibiotics. The disease is primarily an expression of poverty and its consequences, especially overcrowding, and in the Arctic, these are usual. Latent infection endures in almost everyone older than 40. It revives itself regularly and seeps through the community; by the time a new outbreak is recognized there are usually dozens of new infections, some apparent, most already gone dormant.
Therese is 27 and does not know from whom she caught her illness. There are nearly as many possibilities as there are people around her. Half her left lung is taken up by a giant cavity full of the organism. Every time her sputum has been analyzed in the last two years, it has been found to be packed with the little rods of Mycobacterium tuberculosis that stain crimson when examined under the microscope. She coughs constantly and is so thin she is cold even inside, wrapped in blankets. After months of unsuccessful treatment in Arviat, she spent much of last winter in a hospital in southern Canada, but she continued to lose weight steadily. Her sputa remain resolutely positive. Finally, she insisted on going home, to her children, and to the tundra.
She has the cachectic facies of a painting of a Victorian consumptive, Munch’s Sick Child, perhaps. It is an uncomfortable feeling to find in her sickness the conventions of beauty — boniness and pallor. She is suspicious of doctors and nurses and takes her medication only episodically. People worry aloud about her children. This is a catastrophe in formation. A slow-moving freight train.
This catastrophe threatens to erupt on a vastly larger scale than Arviat, to involve the entirety of North America. For the past 12 years I’ve treated patients in TB hot zones such as the Arctic, the Pacific Islands, inner-city America. What I and others on the front lines have to report is that TB is migrating out of these geographically remote or economically isolated communities and into the mainstream.
Perhaps this shouldn’t surprise us. Tuberculosis infection has been so prevalent that for most of human history it was an almost normal, if often lethal, part of the human bio-niche. Hippocrates deemed it the most widespread disease of his time, and almost always fatal. In 1680, John Bunyan called TB “the captain of all these men of death” and indeed, until the development of antibiotics, 1 in 2 people who contracted it died. Between 1850 and 1950 it killed 1 billion people. Modigliani died of tuberculous meningitis, infection of the lining of the brain. Keats, a former medical student, remarked famously on the bright red and foreboding color of his sputum. Chopin, Chekov, Emily Brontë, Robert Louis Stevenson, Orwell, Kafka, Vivien Leigh: all claimed by TB. Then, for a mere 50 anomalous years, the disease ebbed and a lingering cough was no longer cause for immediate terror.
Once antibiotics were mass-produced in the late 1940s, First World transmission rates fell steadily; when latent infections reemerged, they were usually caught and cured. Such hidden reservoirs of TB dwindled as those infected either aged and died of other causes, or were identified through positive skin tests and treated. By the early 1970s, the problem was seen as past, and U.S. public-health authorities charged with monitoring and treating residual outbreaks began losing their funding. Surveillance for TB became more lax, supervision of therapy more haphazard. Such slipshod treatment has led not only to new infections but, more terrifyingly, to the emergence of multidrug-resistant TB strains, or MDR-TB, which a recent Harvard study called “Ebola with wings,” and is now found in the United States and more than 100 other countries.
Several other events have acted to reignite the old problem known as phthisis, consumption, or the white plague (named for the pallor it causes). Just as public-health spending on TB was declining, immigration from areas where the disease has never been much beaten back — from Asia, Africa, and especially from Russia — steadily rose. Despite a decade-long effort mounted by the World Health Organization, the global rate of TB continues to climb about 3 percent a year. Currently, then, 8 million people worldwide fall ill with the disease each year and, because only a quarter receive effective treatment, 3 million die. Furthermore, a third of the world’s population — another 2 billion people — carry latent infection, each of whom has about a 10 percent chance of it activating in their lifetime. When TB does activate, it does so insidiously, often simply as a persistent but infectious cough, and on average, an active case will infect 20 other people before it is identified and treated.
Unless Americans are willing to adopt suffocatingly draconian immigration policies, the likelihood is that with globalization TB will again become epidemic here, in the same way that HIV moved from Africa to take root throughout the world. Suffering does not localize. When we engage with the world, we engage, inescapably and absolutely, with the world’s infections. And the most devastating infection in the world is not Ebola or Lyme disease, West Nile virus or even HIV, but tuberculosis.
Mycobacterium tuberculosis is descended from similar organisms that have inhabited cattle for eons. About 8,000 years ago the organism spread to humans. It has since adapted to us, tweaking its genetic arrangement to optimize its capacity to spread and persist.
Its virulence is largely a consequence of the thick, waxy cell wall that surrounds the organism like a rind, making it substantially resistant to the immune system. When the organism is inhaled, it lodges in the alveoli of the lungs, the little air sacs that exchange oxygen for carbon dioxide within the blood. When the immune system identifies the presence of this foreign protein, it recruits white blood cells called macrophages (“big eaters” from the Greek; one pictures a pie-eating contest) to engulf and bathe the invader with toxic chemicals. Despite the macrophages’ defenses, the creature, because of its thick rind, often survives and slowly replicates itself until each macrophage is so full of tuberculosis bacteria that the cell bursts and dies. The organisms drift on, to be engulfed in turn. Most of the time an equilibrium is attained, nearly as many tuberculosis bacteria are killed as survive, and the spread of the creature is checked. This is the latent phase, and it can go on for decades until for some reason, or no obvious reason at all, the balance is tipped.
The balance might tip because the immune system is weakened by stress, or by pregnancy, or by another infection (especially HIV), or by starvation, or simply by age. In any case, when it does, the bacteria overwhelm the immune system. They begin to fill the adjacent alveoli and block the exchange of oxygen and carbon dioxide. The patient becomes short of breath. The immune system’s efforts to fight off the infection inflame the walls of the lung, which come to bleed easily. The patient develops a fever, and she notices streaks of blood in her sputum. Initially, as Keats knew, this blood will be dark red and venous; later, as infection erodes its way into arteries, it becomes bright crimson. If the affected artery is a large one, this may be what is called, chillingly, a “pre-terminal” event. Katherine Mansfield expired in a great geyser this way.
Even if the artery isn’t large, now the seed is in the wind and the creature in the blood — it swims to every organ system: the brain, the kidneys, the intestines, the bones, the ovaries, the skin, the uterus, the heart. Any medical textbook more than a generation or two old lists tuberculosis as a possible cause of almost any organ dysfunction, and usually high up on that list.
One of the great calamities for all mankind, tuberculosis was simply the worst thing that ever happened to the Inuit, and to indigenous Americans more generally. Nobody knows why it has been so prevalent among them. There are many possible explanations: the small, crowded snow and skin dwellings they lived in; the lung diseases caused by the smoky seal-blubber lamps they lit the iglus with; a genetic vulnerability; and, most persuasively, the chronic, recurrent famine that always lurked on the edge of the ice floes. The Inuit called it puvaluq, or bad lung, and once introduced by Europeans it infected most of the Inuit in the Arctic. Across the continent it killed many thousands — perhaps millions — more Native Americans, largely clearing the Great Plains; when settlers spread across them in the mid-1800s, they often commented on the wide-open and fertile grasslands, uninterrupted by signs of human habitation. But for the creature, the land would have been as it had been only a few years earlier — alive with children and hunters and women growing corn.
The small desperate bands of remaining Plains Indians were herded into crowded reservations that accelerated the contagion process already well under way. In Kivalliq, where I work, the Inuit were compelled by the Canadian government in the early ’50s to move into the dismal little settlements it had erected on the shore of Hudson Bay, largely to facilitate attempts to control the infection. Throughout the ’50s and ’60s, ships with mobile X-ray units visited every summer, and those found to have active disease were evacuated to sanatoriums in the south. Children later returned to their barely remembered parents were often unable even to speak to them, their language lost in the land of drive-in movies. By the late 1960s, the last of the nomadic hunting families had come in off the ice and settled in the clapboard houses provided them by the government, there to begin the cycle of acculturation that continues today.
In the hamlets of Coral Harbour and Arviat, there are now active epidemics. Five years ago it was in Repulse Bay, a few years before that, Chesterfield Inlet. The Inuit’s historic exposure rate to TB was so high that it can be expected to recur reliably for decades to come. TB remains endemic among most Native Americans, with an annual incidence that in 1987, for example, was 400 times higher than among urban Caucasians. Not that resources haven’t been thrown at the problem — in Kivalliq the annual spending per capita on health approaches $15,000.
But tuberculosis isn’t like other communicable diseases that can be cured with a few doses of inexpensive and safe medicine. Like a storm forming from the coalescence of several weather systems, TB is the perfect pathogen in many respects: It has long latent asymptomatic phases, allowing it to dwell on in populations; it is spread invisibly, in the air, so infection-control measures like hand washing have no effect on transmission; and when it takes hold it erodes every single organ system. And its perfection is preserved most of all by its ability to shrug off our medicines within a few decades of their development.
Pools of prevalent tuberculosis infection surround North America from every side, including the islands of the Pacific Ocean, the American possessions of Saipan, Guam, and Samoa among them. The problems of poverty and crowding among the Inuit are echoed on these islands; the only real difference is the temperature, but this ceases to matter to the infected — as the disease progresses, one feels as if on fire wherever one is.
Two winters ago I spent three months working in Saipan, the largest of the Northern Mariana Islands, which rises out of the deepest water on the planet as a long and verdant mountainous ridge. Most people in Saipan live close to the sea, descendants of ancient mariners who undertook thousand-mile-long open-water passages in outrigger canoes, without compasses or maps, as we understand them. A kind of poverty exists there today that did not when the people were less wealthy. The island is more crowded than it ever has been, and rests uneasily between an Asian and an American sensibility. It has the diseases of both existences and the cultural stability of neither — the perfect picture of globalization.
The Marianas are remnants of the Pacific empire that America won from Japan and are now a commonwealth of the United States, like Puerto Rico; those born here are American citizens. Most of the people who live in Saipan are not, however, but rather come here as contract workers for the garment industries on the island, which value the combination of “Made in the usa” labels and cheap labor. The workers migrate north from the Marshall Islands, and west from China, Thailand, and Bangladesh.
Saipan’s TB clinic processes a steady stream of arrivals found to have shadows on their mandatory screening chest X-ray. Legal workers are motivated to comply with their therapy — if not, they are sent home expeditiously. But illegal workers represent a thornier ethical and political problem — as they do throughout the developed world — and one of the principal obstacles to controlling TB. For wherever there is suspicion between public-health authorities (the term itself is illuminating) and the infected, TB thrives. Illegal workers, migrants, intravenous drug users, all of whom dwell in the various demimondes of a fractured society, are among the most likely to be infected by TB. And dwellers of any demimonde recoil instinctively from a stranger’s knock on the door. This is a survival skill.
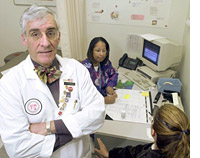
Among Saipan’s indigenous Chamorro — much wealthier and U.S. citizens — TB also endures and flares periodically, not yielding much over time to the efforts of Artin Mahmoudi, who ran the TB clinic. Dr. Mahmoudi examined the DNA from TB strains he obtained from the Chamorro and the migrant workers. Despite the widely held prejudice against the migrants, he found that, for the most part, the TB found among the Chamorro is not acquired from them, but from latent infections that have activated. There is enormous potential here for new strains of TB to burst out of the peeling-paint dormitories that house the migrants. But this has not occurred. Yet. In the meantime, Mahmoudi holds his breath. And wrestles with that dragon, not yet loose.
Mahmoudi is Baha’i, originally from Iran; three family members were killed following the overthrow of the Shah. He is a handsome and graciously mannered man; his personality dominated the hospital on Saipan. This comes across as high-handedness to some. An acquaintance once told me, before I’d met Mahmoudi, “You do have to spend a fair amount of time telling him how smart he is.” It was clear to me, however, that he elevated the standard of Saipan’s medical care far beyond what it otherwise would have been.
His desk, in the office he shared with three other internists, all crowded together just like in a college-dorm study center, was littered with books on the history of TB and CDC reports on new resistant strains. His faith makes him suited for his task; he is part zealot, part missionary. His is the sort of effort that could change the picture of transmission worldwide, but there are no other Mahmoudis anywhere close to here. Elsewhere, in the Marshalls, for instance, TB is simply an observed and not much discussed fact. People cough, they sweat, they die.
Such indifference is a measure of the disease’s intractability. The first effective anti-TB drug, streptomycin, came into use in 1948. By 1950, resistant strains were commonly observed. Other antibiotics were developed in rapid succession, but TB proved fully capable of becoming resistant to any of these agents, and quickly. A strategy was devised to bombard a patient with four drugs simultaneously and then to continue therapy for six months with at least two drugs that the patient shows no resistance to. All such drugs can have debilitating side effects, including color blindness, numbness, deafness. It’s easy to imagine why an Inuit hunter would eschew treatment, why anyone would. In practice, people take the medication reliably as long as they feel unwell, and when they feel better they stop.
Ideally, then, the drugs are administered by a health professional, and their ingestion witnessed. When this approach — called Directly Observed Therapy, Short Course, or dots — is used, resistance is dramatically lessened. But when treatment is sporadic, when dots therapy isn’t pursued until completion — and this is common, even in the United States — resistance becomes inevitable.
The facility with which Mycobacterium tuberculosis develops resistance surpasses that of nearly any other organism; it is one of its defining characteristics. When TB becomes resistant to multiple drugs, the cure rate, even under the best circumstances, falls from 98 percent to 60 to 70 percent. In the Third World, treatment of MDR-TB is so expensive — up to $10,000 per person — and difficult to deliver that the World Health Organization recommends that antibiotics should be dispensed only to patients whose bacteria is still drug sensitive, and then only in the context of a dots program. Unfortunately, dots is not practiced in a third of the world’s nations.
Mahmoudi introduced the dots strategy to Saipan, and with it at least those identified are reliably treated. But the countervailing effects of increased immigration and the rise of chronic diseases among the Chamorro have served to check dramatic progress. The irony in the Pacific Islands is that, though still beset by traditional tropical infections such as malaria, dengue fever, and elephantiasis, the new great killer is the combination of obesity, diabetes, and vascular disease. These diseases of affluence have not so much supplanted the old diseases of deprivation as teamed up with them. Diabetes — epidemic among Pacific Islanders, as it is becoming among the other great traditional maritime people, the Inuit — or any malady that causes immunosuppression, makes TB, aggressive enough in the healthy, vastly more threatening. It is in keeping with its character that TB would find a way in the modernizing Pacific to exploit both the enduring poverty of the area and the consequence of imported and too plentiful food.
I spent my evenings walking along Beach Road, down by the American and Japanese tourist hotels. Just off Beach Road are brothels and massage parlors. The women who work here are garrulous. Most were garment workers but grew tired of minimum wage and breathing cotton fibers all day long. Astonishingly, there is very little HIV here — so far. Everyone knows that is going to change. Mahmoudi just shook his head when he discussed the implications HIV will bring to the problem of TB here.
When HIV emerged 20 years ago, it helped cause the incidence of TB in the continental United States to rise 20 percent among adults and 35 percent among children. But things are far more dire in the developing world: In Africa, for example, tuberculosis is the disease that kills the vast preponderance of AIDS patients. HIV and tuberculosis are almost co-infections — each renders its victims more susceptible to the other. From the moment a person becomes infected with HIV, he is 800 times more likely to suffer activation of latent TB. This is because the type of immunity that aids specifically assaults, called the cell-mediated immune system, is precisely the arm that normally resists TB infection. At the same time, TB imposes a certain type of immunodeficiency on those it infects that renders them far more susceptible to HIV. The twin catastrophes of HIV and TB share far more than geography; they are as intimately complicit in each other’s evil as Leopold and Loeb.
Last August, I traveled from my home on Saltspring Island, British Columbia, to New York on a Cathay Pacific flight that originated in Hong Kong, connecting through Vancouver. The passengers around me were exhausted from the 14 hours they had already spent flying, and the sound of rasping snores filled the cabin, notwithstanding The Royal Tenenbaums and their efforts to distract us. In the orange high-altitude morning light, Gene Hackman barked silently on the bulkhead screen in front of us. Behind me a child coughed steadily, suffering, no doubt, from an innocent viral respiratory-tract infection, or perhaps some sinusitis.
The passengers around me were distinguishable from the men and women I treated in Saipan only by the authenticity of their Rolexes. They appeared to have prospered in China’s economic boom, probably now resident in Hong Kong or Singapore, but the adults were likely born into conditions similar to those of the Saipan garment workers. How many degrees of separation from TB could I possibly hope to be?
I had come to the New York area to see Lee Reichman, who knows and admires Artin Mahmoudi. A former president of the American Lung Association, Reichman is now the executive director of the New Jersey Medical School’s National Tuberculosis Center, where he oversees 78 physicians and nine field-workers. He is 64, has been working with TB for the last 30 years, and is so deeply alarmed that in the fall of 2001 he published Timebomb: The Global Epidemic of Multi-Drug-Resistant Tuberculosis to draw attention to the problem.
One of the reasons that Reichman is held in such high regard is that in the 1970s he was virtually alone in warning American public-health authorities of the disaster that would come if they slashed TB funding. Sure enough, in 1986, thousands of new cases of active TB, many MDR-TB, appeared in U.S cities; in 10 years the rate of new infection increased by 20 percent. Not only was the rate of TB infection increasing, but it was appearing in odd forms — outside the lungs, as meningitis, or in the kidneys, for instance — more frequently than normal. The cause was HIV. Checking this surge cost more than a billion dollars.
But once again, Reichman sees what he calls “the U-shaped curve of concern.” Thinking that they’ve successfully combated the latest TB outbreak, the medical profession is again treating the illness haphazardly. “We know this from the development of MDR-TB,” he says. “Every case of MDR-TB is evidence of inept medical therapy; these strains do not occur naturally.” A study Mahmoudi published found that in 1993 doctors in a Denver hospital made an average of 3.9 treatment errors per TB patient; this poor treatment of an outbreak that began among migrant workers gave rise to a 75 percent increase in Colorado cases — including some that are MDR — in the past three years. “Sadly,” Reichman notes, “little has changed. In the states of Virginia and Washington, TB medications are still not provided free to patients. This represents a violation of every principle of TB care. You have to make it as likely as possible that the patient will take the medicine for the necessary length of time. And the people with the least money are the most likely to have TB.”
We sit in his office in central Newark. He is animated and arch, not as cool as Mahmoudi, more accessible. He is dismayed by the indifference of the public to its own peril, but it is the acquiescent dismay of an older man. He shrugs. There are other problems just as large, right now. He wants to tell me about the Russian prisons.
In Russia there are 1 million men and women in stygian cages, coughing into the close and crowded air. Reichman, who visited the prisons in 1998, thinks that essentially all of them have either active or latent TB by the time they are released. He was flabbergasted by the experience. The treatment that Russian prisons employ is more of a gesture than therapy, and it is a disastrous gesture: occasional dosing with inadequate antibiotics, giving rise to organisms with resistance so broad as to be almost untreatable. It is only one of the horrors of Russian prisons, but it is the one that threatens the world outside those concrete walls.
Every year 300,000 Russian prisoners are released. Then they, and the creature within them, move away, understandably, from those cages, often with some velocity. Inevitably, some are propelled across the Atlantic. Barry Kreiswirth is a microbiologist who works with Reichman. His preoccupation is collecting and categorizing the DNA fingerprints of different strains of TB; he has 16,000 now, the world’s largest collection, he told me with great pride.
In Tomsk, Siberia, is a prison rife with TB, including a strain that arose there called W148 that is almost always resistant to all commonly used anti-TB antibiotics. In March 2000 Kreiswirth was asked to examine a new strain of resistant TB found in New York. It was W148. He was stunned. He contacted the New York Public Health Department. The strain was found in a Russian immigrant. W148 was here. Suffering does not localize.
This example is just one among thousands. The World Health Organization estimates that 50 percent of the world’s refugees are infected with TB. And at least half of all diagnosed TB cases are found among foreign-born people who have moved to industrialized countries. Legal immigrants to America over the age of 15 must have a chest X-ray upon entry. But this does not catch those for whom the disease is not developed enough to show up on film, or adopted children who come with active TB, or business travelers, or tourists, or illegal aliens. In the 1990s, cases among foreign-born Americans rose from 29 percent to 41.6 percent. So it is not surprising that U.S. infections are, thus far, concentrated in areas favored by new arrivals. Strains of TB once found only in Mexico have migrated to Texas. In 2000, some 16,000 people living in the United States developed active TB; half were foreign born, with 1,332 — or 8.3 percent — living in New York City. In 2001, 36 percent of all reported MDR cases were in New York City and California.
But just as it spread from Siberia and Senegal, TB will not stay contained within pockets of America for long. For now it is chiefly found among the marginal and the overcrowded, epidemic, for example, among the homeless and in our prison system, where 2 million Americans reside and 600,000 more work. But prisoners are paroled and guards go home. In 1993, Reichman writes, “one New York county found that 24 percent of identified cases occurred in jail inmates, former inmates, jail employees, or community contacts.”
Fear of MDR-TB has led to a different kind of incarceration. In the last few years U.S. health authorities have committed hundreds of patients to hospitals to ensure that they complete their course of medicine. The notion of treating sane patients against their will is deeply discomfiting to most physicians. The laws that allow for this date from the Victorian era, and the idea seems similarly obsolete. But the fact that this measure continues to be resorted to underscores the threat that MDR-TB represents. There hasn’t been a new class of anti-TB antibiotics developed since the late 1960s; new drugs are estimated to be at least seven years away. Fifty million people have MDR-TB, 2.5 percent of all TB cases. But in certain countries, 20 percent are MDR. And in some places, including in New York City, strains exist that are resistant to all known antibiotics.
Reichman is blunt: “We sit on the edge of a potential catastrophe. Government doesn’t take this problem seriously, physicians do not reliably treat this problem, and the public thinks TB isn’t sexy enough to merit its attention. Ebola kills a couple of hundred people and there are movies about it. TB kills 2 million people a year already, more than hiv and malaria, more than any other single infection. And it is curable and has been curable since 1948. This inattention is just what this infection needs to explode, for the time bomb to go off!”
To the extent that anyone is working to forestall such an explosion, it is people like Rebecca Stevens. She is a field-worker for Reichman, administering dots, and I went with her as she fanned out into central Newark, policing the compliance of 28 patients. There is some irony to this: Both Rebecca and I were previously diagnosed with latent tuberculosis, a troublesomely common affliction among health care workers. We both hope that ours are drug-sensitive organisms. Treatment among latent patients is always speculative as it is impossible to test them for drug sensitivity. It is conceivable that one day either Rebecca or I might find ourselves with a Rebecca in our own lives, dropping by to watch us take our pills.
We visit the apartment of sisters Chariesse and Mona Greene, and the nine children they care for between them. The kids range from five months to 10 years; six have developed TB. Chariesse is sick, and weighs 94 pounds, even less than Therese Oopik. Out of the hospital for a week, she is tired and worried about her infant niece, who is still hospitalized with tuberculous meningitis. Rebecca says the child does not look well.
Mona had tuberculous meningitis when she was 12, she tells me. Chariesse may have caught TB from Mona at that time, or even years earlier. It is not possible to know. The children probably caught TB from Chariesse. Another boy Mona babysits is in the hospital, too. He’s doing better than her niece.
I tell her I’m glad. She nods. She hollers at one of her daughters for not picking up her clothes. Rebecca yells back that the hollering is giving her a headache. The house quiets as Rebecca mixes the drugs in with jam for the younger children. The children ask Rebecca for their cans of Boost, a dietary supplement she brings them when she visits. “Mona is what keeps this situation together,” Rebecca tells me privately. “Viewed from their own situation, they’re doing okay. From my situation, or yours, maybe not, but from theirs, they’re all right.”
The apartment has a manic, agitated quality to it; the children are both excited by visitors and shy. Chariesse and Mona are in their 20s, and seem embarrassed about the chaos around them. Both have had drug problems on and off for a long time. Currently not, they say, and Rebecca is inclined to believe them. Chariesse is too sick, and since she got sick, everything pretty much falls to Mona. Things are going too well, Rebecca says, for Mona to be using much.
Too well is not that well, really. They are being evicted. The $800 in welfare they receive is not enough to pay for both food and the apartment they live in, where rats leap from the cupboards when doors are opened too quickly. Mona and Rebecca have a long conversation about the homeless shelters in the area. There are boxes stacked along the living room wall, ready to move their few possessions, and clothes and mattresses on the floor. As we prepare to leave, to distribute the antituberculosis medications to other patients, Mona says she doesn’t know how they are going to do it, where they will live.
The last time I saw Therese, she told me she tried not to think about the future, about how all this would end. She enjoyed being home and tasting the Arctic char. The snow would melt soon, and there would be walrus and beluga whale to eat. She knew the peace wouldn’t last. And it won’t.